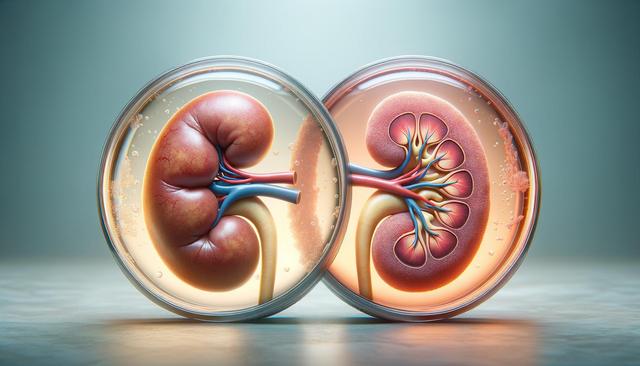
Visual Comparison: Healthy vs. Unhealthy Kidneys
Understanding the visual difference between a healthy kidney and an unhealthy one can be a powerful step in raising awareness about kidney health. A healthy kidney typically appears smooth, bean-shaped, and has a consistent reddish-brown color due to rich blood supply. In contrast, an unhealthy kidney may show signs of scarring, shrinkage, or abnormal texture, often appearing pale or blotchy. These visual cues are not just surface-level differences—they reflect underlying issues such as chronic inflammation, fibrosis, or reduced blood flow. Medical imaging tools like ultrasound, CT scans, and MRIs often help doctors detect these changes early, especially in individuals with risk factors such as high blood pressure or diabetes.
When kidney damage progresses, the organ may lose its ability to filter waste and fluids effectively, leading to visible structural changes. For example, polycystic kidney disease can cause the kidneys to enlarge and develop fluid-filled sacs, while chronic kidney disease (CKD) leads to gradual shrinkage and hardening of tissues. Recognizing these changes is crucial, especially in the context of evolving treatment options like those listed under “FDA-Approved Kidney Medications for 2025: Full List & Updates” which are designed to slow or reverse kidney damage when detected early.
New Kidney Disease Medications in 2025: What’s Changing
Recent advancements in nephrology have led to the approval of several new medications targeted at treating CKD and related conditions. These medications have gained attention in the medical community not only for their effectiveness but also for offering improved safety profiles and fewer adverse effects compared to older drugs. In 2025, the FDA has approved a new generation of SGLT2 inhibitors, mineralocorticoid receptor antagonists, and endothelin receptor antagonists. These therapies aim to reduce proteinuria, slow kidney function decline, and manage comorbid conditions like heart failure and diabetes.
Among the key changes in treatment protocols this year are:
- Earlier introduction of pharmacologic therapy for patients at risk of rapid CKD progression
- Combination therapies tailored to patient-specific conditions and genetic markers
- Increased use of telemedicine to monitor drug efficacy and side effects in real time
These developments align with the keyword “Chronic Kidney Disease (CKD) Treatments: What’s New This Year” as they reflect a significant shift in how CKD is managed from the early to advanced stages.
Prescription vs. Over-the-Counter Options for Kidney Health
When it comes to supporting kidney function, patients often wonder whether over-the-counter (OTC) supplements are sufficient or if prescription medications are necessary. While certain OTC products such as phosphate binders or vitamins like B-complex may support kidney health in early stages, they are no substitute for prescription-strength therapies approved by regulatory bodies. The keyword “Prescription vs Over-the-Counter Options for Kidney Health” becomes particularly relevant here, as new guidelines in 2025 emphasize the importance of clinician-monitored treatments for effective disease management.
Prescription medications are typically recommended for patients with moderate to severe CKD or those experiencing rapid decline in kidney function. These may include:
- ACE inhibitors and ARBs to control blood pressure and reduce proteinuria
- SGLT2 inhibitors to manage blood sugar and protect kidney function
- Newly approved anti-fibrotic agents that target kidney scarring
While OTC options might offer supportive benefits, they lack the targeted action and clinical validation of prescription drugs, making them unsuitable as standalone treatments for CKD.
Comparing New Kidney Drugs: Effectiveness and Cost
With multiple new FDA-approved medications entering the market in 2025, patients and healthcare providers are increasingly interested in comparing their performance. The phrase “How New Kidney Drugs Compare: Effectiveness & Cost” encapsulates this growing concern. Effectiveness is often measured by a drug’s ability to slow the decline in estimated glomerular filtration rate (eGFR) and reduce albuminuria, while cost considerations include insurance coverage, availability of generics, and patient assistance programs.
Some of the new drugs show promising results in clinical trials by:
- Reducing hospitalizations due to kidney-related complications
- Delaying the need for dialysis initiation
- Improving quality of life scores in patients with advanced CKD
However, these benefits come with varying price tags. Tiered insurance coverage means that not all patients will have equal access to the newest medications. Additionally, the introduction of biosimilars and generics is expected to make certain therapies more affordable by late 2025, but until then, cost remains a barrier for many.
Managing Side Effects: What Patients Should Expect in 2025
While new medications offer hope, managing side effects remains a critical aspect of CKD treatment. The keyword “Managing Side Effects: What Patients Should Expect in 2025” is relevant as more patients begin using these newly approved drugs. Common side effects in kidney medications include electrolyte imbalances, gastrointestinal issues, and increased risk of infections, particularly with immunosuppressive therapies.
Healthcare providers are now placing greater emphasis on:
- Routine monitoring of blood and urine parameters
- Patient education on recognizing early signs of adverse reactions
- Adjusting dosages based on individual tolerability
Digital tools such as mobile health apps and wearable devices are also being integrated into care plans to provide real-time data on patient health, enhancing early detection and intervention. As more information becomes available on these medications throughout the year, patients are encouraged to maintain open communication with their healthcare teams.
Conclusion: Proactive Kidney Health in a New Era of Treatment
The visual and functional differences between healthy and unhealthy kidneys highlight the importance of early detection and timely intervention. With the arrival of new FDA-approved therapies in 2025, individuals living with or at risk of CKD have more options than ever before. By understanding the benefits and limitations of both prescription and OTC products, comparing drug effectiveness and cost, and preparing for possible side effects, patients can make informed decisions in partnership with their healthcare providers. As the field of nephrology continues to innovate, staying updated on “FDA-Approved Kidney Medications for 2025: Full List & Updates” and emerging treatment trends is essential for maintaining kidney health and improving long-term outcomes.


Leave a Reply